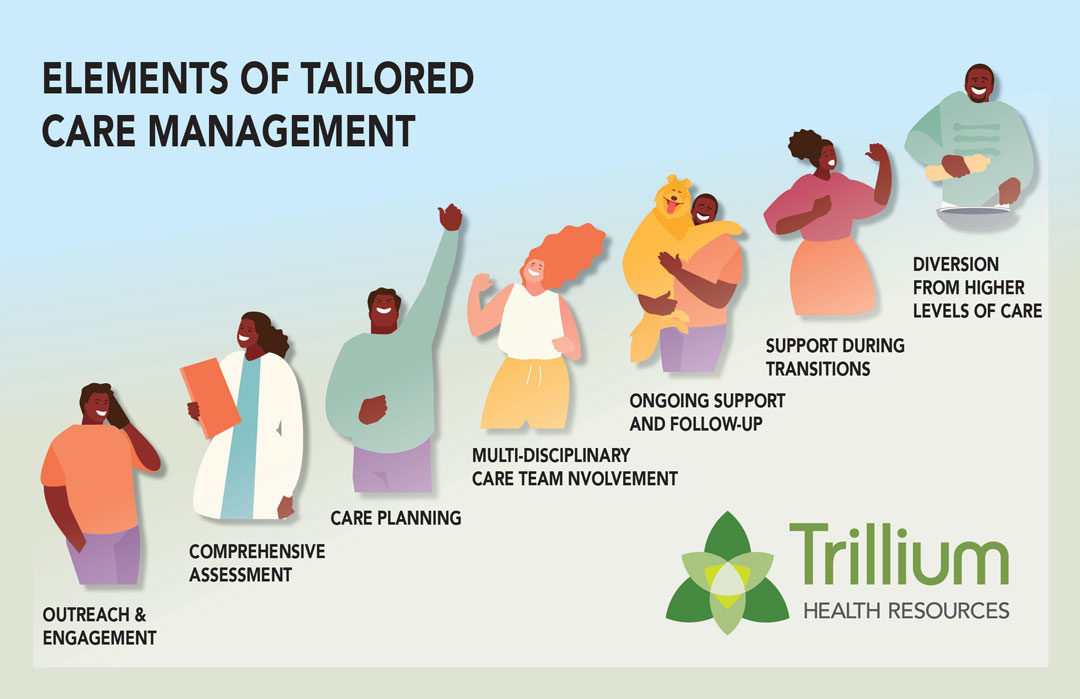
Elements of Tailored Care Management
All members in Tailored Care Management, no matter where they receive it, will have access to the following:
- Care management staff will contact the member to introduce themselves and answer questions.
- Staff will collect information about all of the member’s needs: physical and behavioral health, medications they are taking, social support, advanced directives and more.
- Staff will develop a care plan that will include all the details collected during the comprehensive assessment.
- All the health care providers working with the member will make sure the care plan puts the member at the center of everything and that any plans of action best support the member.
- Regular communication to share about progress towards member’s goals.
- Talking with staff at various settings and services as member’s needs change.
- Telling members about community-based services, putting them in touch with those services, helping with needs such as housing, and developing and implementing a Community Integration Plan.
All Trillium Tailored Plan Medicaid members are enrolled in Tailored Care Management except for:
- Members in Assertive Community Treatment (ACT);
- Members in Intermediate Care Facilities for Individuals for Intellectual Disabilities (ICF-IIDs); and
- Members in the High-Fidelity Wraparound program.
Page last verified on